Ever since the invention of electronic communication devices physicians have used technology in the care of patients, practicing “medicine at a distance”: In the 1950s, the Mayo Clinic in USA received an electronically transmitted EKG from Australia; astronauts were telemetrically monitored in space in the 1960s; and the 1970s saw an early emergence of telemedicine to Indian reservations to improve their access to healthcare. In the 1990s, the digitization of radiological images enabled the interpretation from virtually any location in the world and teleradiology was born. Especially over the last 10 years, as technology has become more affordable and reliable, telehealth has moved into the mainstream, especially in the US. This article, based on the author’s experience of working in the field in the US for over 15 years, depicts successful examples of today and examines common applications of telemedicine, while discussing their merits and benefits.
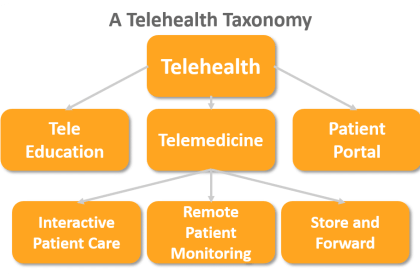
The most common definition for Telehealth is the “delivery of healthcare at a distance” which encompasses online patient education and giving patients access to their health information via patient portals. Telemedicine, as a subset of telehealth, is defined as “practicing medicine at a distance”, i.e., healthcare providers examining, observing, consulting, and treating patients. As illustrated in the Telehealth Taxonomy, the three main modalities by which Telemedicine is practiced include:
- Interactive Patient Care (IPC) – live, interactive communication between a provider and a patient, i.e., secure consults, visits, and exams over video, voice, or text
- Remote Patient Monitoring (RPM) – periodic, asynchronous, or continuous monitoring and transmission of vital signs, including weight, blood pressure, oxygen saturation, glucose levels, heart rate, or heart rhythm
- Store-and-Forward – asynchronous capture and transmission of images, video and sound, e.g., faxing EKGs, sending pictures of melanomas, and teleradiology.
Simply put, Telehealth offers an alternative way to delivering healthcare and practicing medicine. The only difference to traditional care is that the patient and the physician (or other providers, educators, or therapists) are not at the same physical location. Telehealth thus gives patients easier access to care, while enabling physicians to share their expertise beyond their physical location.
The 9 most common Telemedicine Services in US
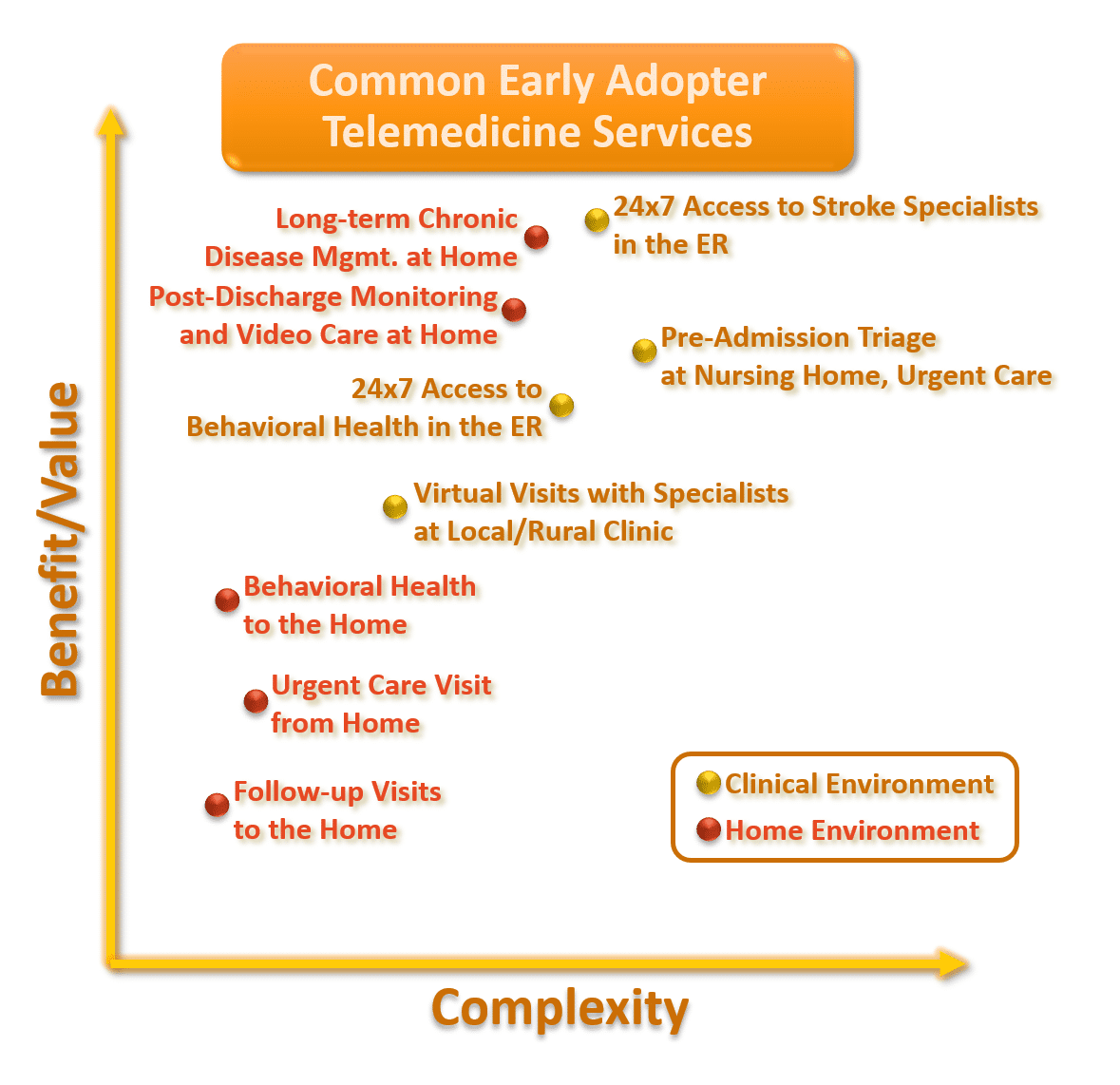
Chart: The nine most commonly deployed telemedicine services in US organized by the complexity of the technology and implementation and their relative benefit and value related to health outcomes and cost savings.
Within the home environment, telemedicine can provide rural or less mobile patients access to primary care and specialty care, especially behavioral health, typically as pre-scheduled appointments. But also ad hoc access to care is easily set up, especially by using external telemedicine service providers who specialize in 24×7 urgent care. A second and highly beneficial set of telemedicine services in the patient’s home involves remote patient monitoring – either for preventing avoidable readmissions for many common (and costly) indications such as CHF or COPD or for the long-term monitoring of chronically ill patients (e.g., diabetes, cardiac diseases) to avoid unnecessary hospitalizations. Within the clinical environment, the highest value and most commonly implemented use cases involve access to a neurologist for stroke evaluations in the ER or remote pre-admission assessments and triage with patients at nursing homes. In addition, especially in rural clinics, access to specialty care provider greatly eliminates the need for patient travel in many situations. The following use cases give a deeper insight into nine most commonly deployed telemedicine services in US, ranging from remotely caring for patients in their home to providing specialty expertise between disconnected healthcare locations.
Telemedicine within the Home Environment:
- Follow-Up Visits at Home: Most outpatient interactions with physicians today are limited to a handshake and a good conversation. So why not spare patients the trip to the doctor’s office? If the physician wants to review test results with a patient or if a patient wants to check in with a specialist on some questions, it can be done just as easily from the patient’s tablet, computer or smartphone at home, in the office or even from the hotel room while traveling for business or leisure.
- Urgent Care Visits from Home: Oftentimes what ails us – a common cold, a headache, or an upset stomach – can easily be addressed and treated with some simple care recommendation or an easily obtained prescription. Obviously, many urgent care conditions cannot be treated virtually – but access to this service can also serve as triage – should I call an ambulance, go to the ER or see my GP the next day?
- Behavioral Health Visits at Home: There is strong correlation between mental health disorders including depression, eating disorders, or low self-esteem and associated diseases such as obesity, hypertension, diabetes, and cardiovascular diseases. Thus, especially regular access to behavioral health visits is key to managing a person’s overall health. Plus, it removes common barriers and root causes of missed in-person appointments.Telemedicine offers a secure, easy solution to connect patients with providers.
- Post-Discharge Monitoring and Video Care: The one-time reimbursement for an episode of care has led many hospitals to seek the prevention of avoidable readmissions by monitoring the patient’s vital signs for the weeks past discharge. Some hospitals have seen readmission rates drop by 80 percent and investments into the monitoring have yielded ROIs of over 1,000 percent.
- Long-term Chronic Diseases Monitoring: Especially for patients with multiple chronic diseases long-term monitoring can bring significant benefits for the patient, the patient’s family, and the care providers. Through periodic monitoring and interaction via video, the decompensation of a patient’s condition, especially when compared to a baseline, can be detected very early and be improved simply through medication adjustments or ambulatory interventions.
Telemedicine within the Clinical Environment:
- 24×7 Access to Stroke Specialists in the Emergency Room (ER): When a patient experiences a stroke, the quicker the life-saving treatment tPA can be administered, the better the health outcome and the lower the treatment cost. With telemedicine, the on-call neurologist can interview the patient, review the CT scanand be exam the patient using a high-definition pan-tilt-zoom camera to search the patient’s face for the stroke-typical drooping of the facial muscles before working with the ER staff to initiate the right course of treatment.
- 24×7 Access to Behavioral Health in the ER: In many American ERs, oftentimes rooms are occupied by mentally unstable patients that must be kept under observation, pending a psychiatric evaluation. 24×7 access to Behavioral Health specialists improves access and keeps the ER’s capacity up and the risk for other patients and staff down.
- Pre-admission Triage at Nursing Homes and Urgent Care Centers: Unnecessary admissions, sometimes motivated by reducing the organization’s liability, sometimes due to the lack of clinical expertise, account for a high percentage of avoidable care cost. With a quick remote assessment and triage of a patient’s condition, avoidable transportation and acute care cost can be avoided or in many cases lead to a direct admission to the hospital, avoiding a costly stay in the ER.
- Virtual Visits with Specialists at Local Clinic: For many patients in rural areas access to specialists oftentimes brings with it the hassle of a multi-hour drive. With telemedicine, specialists can now easily make a “house call” at the patient’s local clinic. And with the availability of many basic exam tools as a digital version, such as video otoscopes and digital stethoscopes, even basic exams can be conducted with the help of a clinically trained telepresenter. Virtual visits with specialists allow patients to learn about treatment options, prepare for procedures or receive post-operative follow-up care.
Just a quick glance at the healthcare systems in the US, Canada, and Scandinavia reveals that telemedicine in the not-so-distant future will become the default way to receive care. Positioned at the intersection of value, convenience, and quality, telehealth is here to stay until the day we all have implantable Tricorders measuring and treating our diseases.
Autoren des Beitrags
Christian Milaster
Christian Milaster is the founder and president of Ingenium Healthcare Consulting.